To explore more Coffee Conversations with Scientists episodes, click here.
Having a baby is a significant health milestone for women of all ages and backgrounds, impacting a woman’s physical and mental health in both the short and long term. High-quality healthcare and access to health education and resources are critical to a woman’s likelihood and ability to have healthy and successful pregnancies and lives afterward. However, certain health conditions and socioeconomic factors contribute to maternal morbidity and mortality, with significant disparities across communities.
In a recent Coffee Conversations with Scientists episode, Anna Palatnik, MD (Obstetrics and Gynecology), discussed the science behind maternal morbidity and mortality, what causes maternal health disparities, and what is being done to improve maternal healthcare for all women.
What Are Maternal Morbidity and Mortality?
Maternal mortality refers to death during pregnancy or death within a year of pregnancy caused by or related to the pregnancy. Maternal morbidity is any health condition attributed to pregnancy that impacts a woman’s health and well-being.
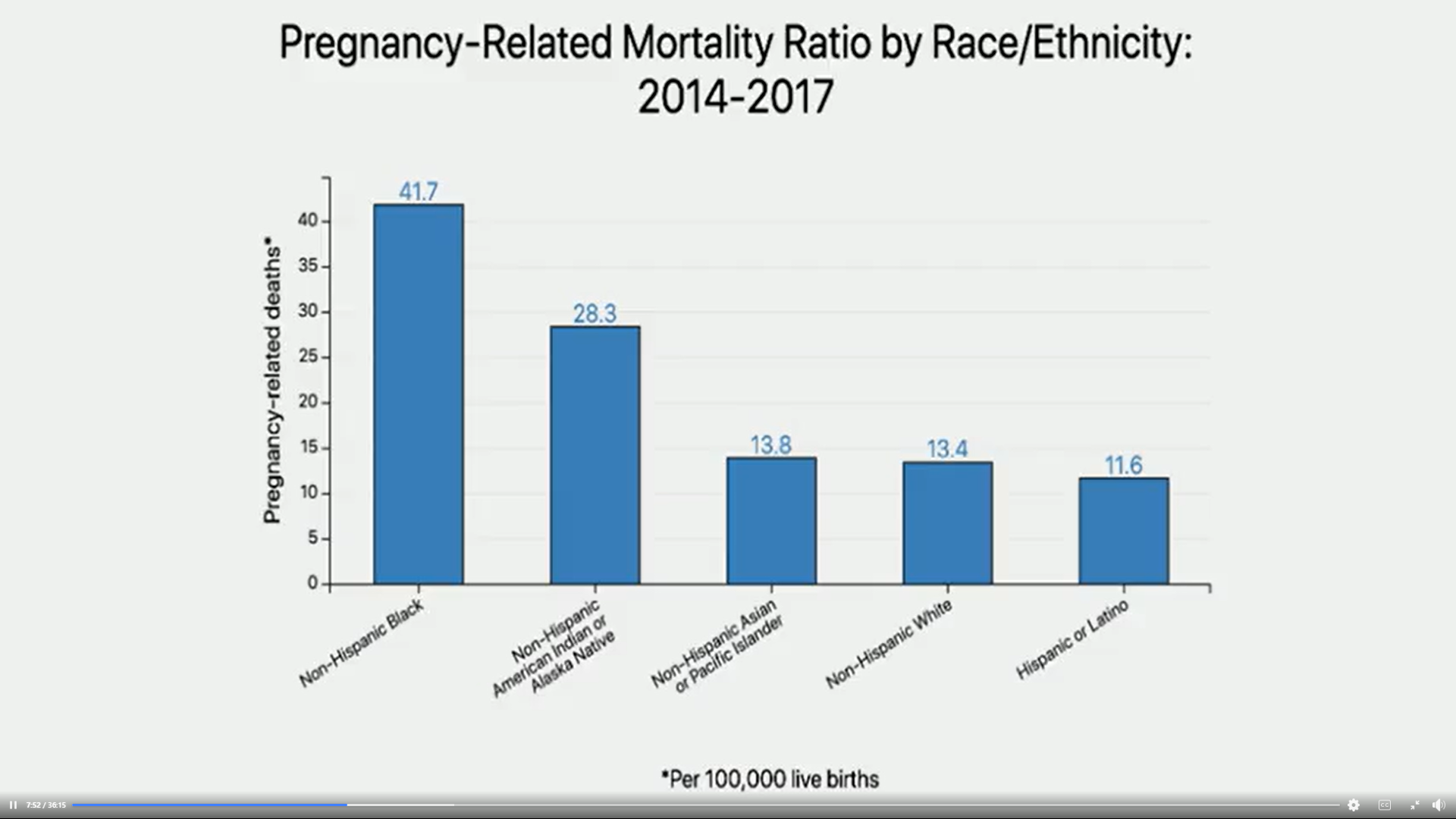
In Wisconsin, the ratio of pregnancy-related deaths to live births is 5.9 deaths for every 100,000 live births. One out of every 100 delivery hospitalizations results in severe maternal morbidities, such as renal failure, eclampsia, and sepsis. For both maternal mortality and morbidity, non-Hispanic Black women experience higher death rates and health complications than White women.
(Source: Coffee Conversations with Scientists – The Science Behind Maternal Morbidity)
The rising rate of maternal mortalities and morbidities and the increasing disparities in maternal health are strong indicators that there is much work to be done to improve maternal healthcare in Wisconsin and the U.S.
Dr. Palatnik noted, “A lot of progress has been made in improving maternal health, but still, many women start pregnancy with suboptimal health and many experience complications, both medical complications and obstetric complications in pregnancy and childbirth.”
What Causes Disparities in Maternal Mortality and Morbidity?
There are various reasons for the significant disparities that exist in maternal health in Wisconsin and the U.S. As Dr. Palatnik explained, they include:
Patient Factors
- Social environment
- Socioeconomic position
- Ethnicity
- Health pre-pregnancy
- Behaviors
Community and Neighborhood Factors
- Social network
- Access to stable housing
Provider Factors
- Knowledge and experience
- Implicit and unconscious bias
- Communication skills and training
System Factors
- High-quality care access
- Structural barriers and racism
- Social and political policies
A combination of these factors and elements such as chronic illness or pregnancy complications contribute to morbidity and mortality. “Many of the disparities can be attributed to low socioeconomic status. If someone struggles to manage their basic daily needs, they can’t prioritize routine doctor visits and taking medication,” said Dr. Palatnik.
What Can Be Done to Reduce the Disparities and Improve Maternal Health?
The issues of maternal mortality and morbidity and disparities in maternal health are complex: There is no simple solution. However, many efforts are being made to address and improve maternal health and maternal health disparities at the patient, provider, and system levels.
Healthy Patient Diet and Lifestyle
During her episode of Coffee Conversations with Scientists, Dr. Palatnik discussed how working toward a healthy diet and lifestyle is an essential first step for patients to achieve health before pregnancy and improve post-pregnancy health outcomes. “Diet plays an important role in postpartum health, especially for patients with hypertensive disorders of pregnancy (HDP). Keeping a good diet and reducing the intake of processed foods can, in my opinion, adjust the trajectory of long-term cardiovascular disease.

Improving Maternal Healthcare Policies
In efforts to reduce maternal health disparities, organizations such as the American College of Obstetricians and Gynecologists and The Society for Maternal-Fetal Medicine promote policies to address the core underlying issues of this problem. Perinatal Quality Collaboratives also have teams that address healthcare processes requiring improvement and change.
Increasing the Quality of Maternal Health Practices
According to Dr. Palatnik, at Froedtert & the Medical College of Wisconsin, healthcare providers undergo education to specifically address and reduce maternal health disparities, including topics such as shared decision-making with patients, implicit bias awareness, and effective patient communication. Standardized protocols and checklists have been introduced to ensure that each patient receives the same-quality labor and delivery care. As Dr. Palatnik said, “When there aren’t guidelines, there’s room for bias.”
Froedtert & the Medical College of Wisconsin providers are partnering with community organizations, such as the African American Breastfeeding Network and the Wisconsin Doulas of Color Collective, to improve support during prenatal care and postpartum and to diversify the prenatal and postnatal workforce. “We’re actively working to avoid operating in silos, partner with organizations who care for pregnant patients, and educate people who might become pregnant... In general, supporting the concept of planning a healthy pregnancy before pregnancy starts.”
Developing Pipelines to Increase Diversity
Research has shown that a diverse healthcare workforce improves healthcare outcomes. Accordingly, Dr. Palatnik shared that efforts are underway to develop pipelines to increase diversity among physicians, nurses, and maternal health researchers. “We know diverse teams perform better and learn from each other.”
Postpartum Remote Monitoring
To ensure that all patients, regardless of location or access to in-person care, receive high-quality postpartum care, Dr. Palatnik advocates for remote postpartum monitoring. Postpartum monitoring, or gathering essential health data—such as blood pressure—is especially valuable for postpartum patients who have experienced preeclampsia or other HDPs. This care option allows for health complications in the first several weeks postpartum to be caught and addressed, which is an important step in improving postpartum care.
Find Out More About Maternal Health
To hear more about the science behind maternal health, tune into the Coffee Conversations with Scientists episode with Dr. Palatnik here:





