Aphasia: New hope for improving language recovery after a stroke
June 2, 2022 Posted by AHW Endowment
To learn more about this funded project, click here.
A mild electrical current that painlessly alters brain cell communication while patients do language exercises may help them recover from aphasia, a disorder that occurs when a stroke or brain injury damages parts of the brain responsible for language, a research project supported by the Advancing a Healthier Wisconsin (AHW) Endowment suggests.
Stroke is the largest contributor to disability among neurological and psychiatric disorders. But research is surprisingly limited for methods to improve language recovery among the 30% of stroke survivors whose daily lives are devastated by aphasia, say researchers from Medical College of Wisconsin (MCW) and University of Wisconsin-Milwaukee (UWM) involved in a $283,737, three-year AHW project that started in July 2021.
Aphasia impairs the ability to speak, read, write, and understand what others say because of damage typically to the left side of the brain. About 1 in 250 people in the U.S. currently have aphasia – roughly 2 million total -- and nearly 180,000 Americans acquire it each year, according to the National Aphasia Association.
Tremendous changes in the brain following a brain injury help the brain recover in the first six months, but for the roughly 20% of stroke survivors who don’t recapture full language and communication abilities, more effective rehabilitation methods are needed, researchers agree.
“It is a prevalent problem that is not adequately researched or funded by NIH because of low public awareness and advocacy for it,” said the AHW project's principal investigator, Dr. Jeffrey Binder, a professor of neurology at MCW and clinical neurologist who specializes in stroke diagnosis and management.
The AHW-supported, double-blind, randomized clinical trial enrolling 40 patients over three years is expected to provide the first detailed, large-scale assessment of a combination of the most advanced method of tDCS (transcranial Direct Current Stimulation) and two process-specific language exercises.
The noninvasive tDCS sends a mild electrical current through the scalp to brain tissue. The current subtly alters electrical communication between brain cells, or neurons, responsible for the brain’s ability to learn. When tDCS is given at the same time a patient tries to learn something new through language exercises, researchers believe neurons may form new connections more quickly.
The first language exercise in combination with tDCS focuses on retrieving what patients know about the sounds of a word they are trying to say (beginning and ending sounds, number of syllables, similar sounding words). The second exercise focuses on what they can retrieve about meaning of the word (appearance, location, or function of the object to which the word refers).
The project brings together experts in stroke, aphasia, human brain language networks, advanced brain imaging, and noninvasive brain stimulation methods. In addition to Dr. Binder, the team includes co-investigators Dr. Sara Pillay and Dr. Priyanka Shah-Basak, both assistant professors of Neurology at MCW, and Dr. Sabine Heuer, an associate professor of communication sciences and disorders at UWM, as well as Dr. Aniko Szabo, an MCW biostatistician.
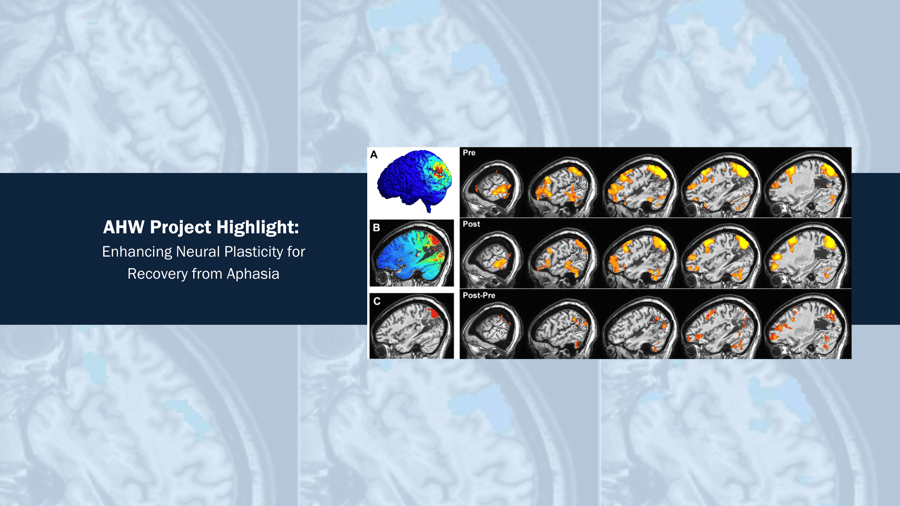
“While the study is in its early phase, preliminary data show lasting changes in functional connectivity – how much different brain areas communicate with each other – months after the electrical stimulation and language exercises”, Dr. Binder said. Brain MRIs are done before treatment and then 10 weeks after treatment.
“No existing, published studies combine tDCS with the two process-specific language exercises in this study”, Binder said.
“So far, we have seen proof of concept, showing promise,” said Dr. Shah-Basak of MCW, who also is a biomedical engineer with expertise in electrical brain stimulation.
The team is using basic science knowledge about language networks in the brain to develop treatment protocols, and state-of-the-art neuroscience imaging that targets specific brain regions that are part of the language network. Multiple regions of the brain try to relearn or function after a stroke. One may interfere with another that contributes to recovery, so pinpointing the contributing region with electrical current is the goal. Individual brain anatomy also varies, and researchers can scan each participant's brain to individualize the area targeted for stimulation, said Dr. Pillay.
“Not everyone’s brain is the same shape,” Dr. Pillay said. “The lesion – the area damaged by the stroke – may be different.”
“Electrical brain stimulation currently is not part of the standard of care for stroke survivors, and generally is not covered by insurance. But we hope that demonstrating benefits of intensive programs with targeted therapies will change that,” Dr. Binder said.


.png?width=300&name=Caregiver%20Roundup%20Blog%20Featured%20Image%20(2).png)
